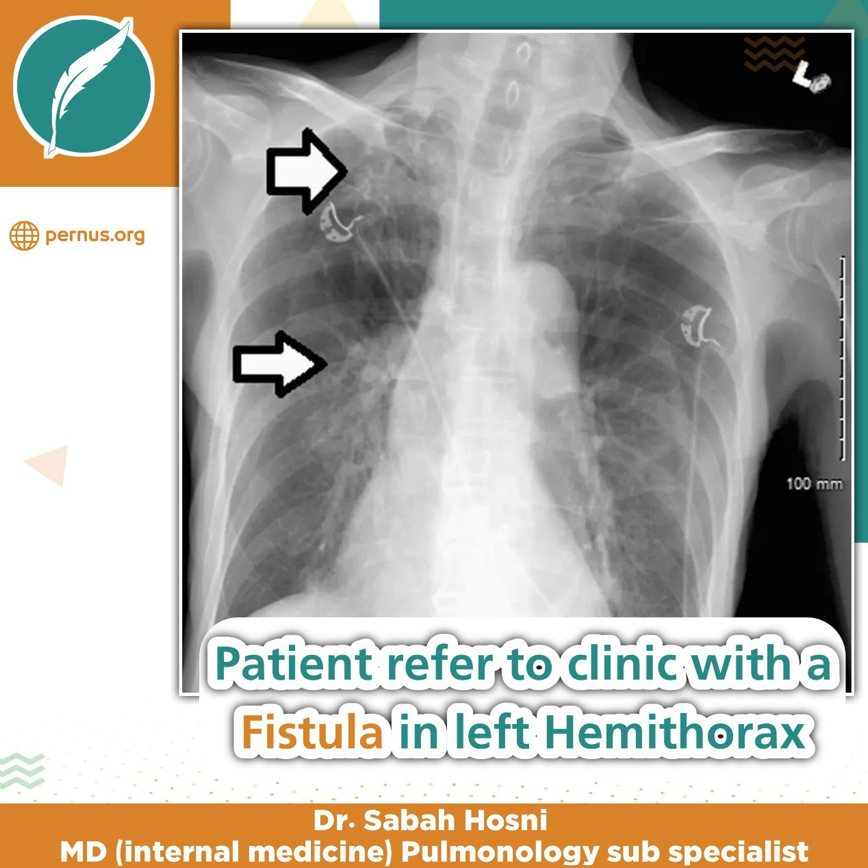
Patient refer to clinic with a Fistula in left Hemithorax
بڵاوکردنەوە:
ڕاستی عبداللە ڕەزا
نووسەر:
د. سەباح حوسنی
بینراو:
392
بەش:
زانست
(PATIENT PRESENTATION)
Patient refer for evaluation by surgeon: -
Patient was male. He was 62 years old.
He had a fistula in left sided of Hemi Thorax with purulent discharge that He should change its bandage three Times a day.
He had not fever and chill, and He had loss of appetite and Weight loss.
He had not hemoptysis a cough and sputum.
(PAST MEDICAL HISTORY)
He was Exsmoker.
He had 30 pack years smoking history.
He had history of pulmonary Tuberculosis disease seventeen years ago.
He was gotten tuberculosis drugs six months and He had negative sputum culture at the end of treatment.
He was history of upper Endoscopy because of Upper GI Bleeding three years ago.
Then He was Admitted to Hospital with Massive Hemoptysis.
● He was undergone more and Antibiotic therapy but patient had continuous purulent discharge.
● He usually was taken quinolone.
● Left lower lobe. Flixibe Bronchoscopy was done for Him. He had massive bleeding from left lower lobe.
● Patient refer to thoracic surgery unit. He was undergone emergent surgery.
● Left lower lobectomy was done.
● He was discharged without symptom.
● Patient had continuous purulent discharge through thoracic unhealing fistula.
● He refers to Infectious disease Specialist.
(PHYSICAL EXAMINATION)
● He is cachectic. He has BiTemporal Atrophy.
● BP:120/80mmhg, PR:70, TR:37.2©, RR:18
● ORAL CAVITY NL
● NECK NL
● CHEST
● A FISTULA was seen in lower portion Anterior Axillary line.
● TACTILE FERMITUS and VOCAL FERIMITUS was decreased in lower anterior left hemi thorax and posterior left Hemi thorax.
(ETIOLOGY)
● lung resection surgery.
● (pneumonectomy, lobectomy, segmentectomy), with a frequency ranging from 4.5 to 20 percent after pneumonectomy and…
● 0.5 to 1 percent after lobectomy.
Thoracic Fistula Differential diagnosis
● infection Most patients present in the first two weeks early (<14 days).
● late postoperative period (>14 days).
● Tuberculosis.
● Non tuberculosis mycobacterium.
● Bacterial infection.
● Malignancy.
(RISK FACTORS)
● Right-sided surgery
● Pneumonectomy
● Chemotherapy and radiation therapy
● Diabetes mellitus
● Heavy smoking and chronic obstructive pulmonary disease
● Low nutritional status or poor wound healing
● Previous ipsilateral thoracotomy
● Residual tumor at the bronchial margin
● A large diameter bronchial stump (>25 mm)
● Extensive lymph node dissection
● Older age (>60 years)
● Prolonged postoperative mechanical ventilation
(THORACIC FISTULA DIFFRENTIAL DIAGNOSIS)
● infection Most patients present in the first two weeks early (<14 days).
● late postoperative period (>14 days).
● Tuberculosis
● Non tuberculosis mycobacterium
● Bacterial infection
● Malignancy
(DIAGNOSTIC EVALUATION)
● Clinical,
● Radiographic
● Bronchoscopic findings
* The image of (Spiral Lung CT Scan)
(SPIRAL LUNG CT SCAN)
● Loculated left sided pleural effusion
● An air fluid cavity in left lower lobe
● Cystic Bronchiectasis in lingual and apical segment
● Fibro nodular pattern in RUL and RML
● Tree in buds in RUL
** The image of check....
(BRONCHOSCOPY)
● Bronchoscopy is critical for the diagnosis and localization of BPF
(NONTUBERCULOUS MYCOBACTERIA) (NTM) SPECIES
● other than those belonging to the Mycobacterium tuberculosis complex
● M. tuberculosis, Mycobacterium bovis, Mycobacterium africanum, and Mycobacterium microti
● free-living organisms
(PULMONARY DISEASE)
● Mycobacterium avium complex (MAC),
● Mycobacterium abscessus
● Mycobacterium kansasii.
● Mycobacterium xenopi,
● Mycobacterium malmoense,
● Mycobacterium szulgai,
● Mycobacterium simiae
(M. SIMIAE)
● isolation at first seemed restricted to the southern USA, Israel and Cuba
● present in the environment and can contaminate medical equipment and laboratory samples
● fewer than 25 percent of M. simiae isolates are thought to be clinically significant
(CHEST RADIOGRAPHY)
● showed infiltrates (54%)
● pre-existent emphysema (25%)
● fibrosis (25%)
● suspected malignant lesions (11%).
(COMMONLY USED DRUGS)
● rifampicin,
● ethambutol,
● ciprofloxacin
● clarithromycin
Regimen selection
● We suggest a three-drug combination:
● Azithromycin 250 to 500 mg daily (or clarithromycin 1000 mg daily) PLUS
● Moxifloxacin 400 mg daily PLUS
(MANAGEMENT AND PROGNOSIS)
BPF
● Chest tube (minimize suction)
● suction (5 to 10 cm H2O)
● Broad spectrum intravenous antibiotics
● Intrapleural fibrinolytic therapy may be appropriate for patients with infected multi-Loculated
● Postural drainage
● The patient should be able to expectorate
● Complete drainage of chest cavity and chest tube drainage should be <30 mL/day
● Technique is done with concomitant pleural irrigation
● Maximize nutrition and treat medical comorbidities
(SURGICAL REPAIR)
● revision of the stump with debridement of necrotic tissue,
● suture reclosure of the bronchial stump with vascularized flap tissue such as omentum or muscle
(PATIENTS NOT SURGICAL CANDIDATES)
● BPF who are high risk for surgery
● eg, suppurative pleuropulmonary disease, hemodynamic instability, severe hypoxemia
(FISTULAS 8 MM)
● fistula closure with airway stents, coils, or Amplatzer devices are options in patients with larger BPFs
● Occlusive materials
● Sclerosants
● Ablative therapy – Argon plasma coagulation
● Endobronchial valves
(REFRACTORY PATIENTS)
● An Eloesser flap is a Ushaped incision and the resection of a number of subjacent posterolateral ribs
Participants:
Hozak Qadir Baram
Bestun Luqman Arif
Shabang Nuraldeen
Supervisor: Dr. Sabah Hosni
MD (internal medicine)
Pulmonology sub specialist
بابەتی هاوشێوە
زۆرترین بینراو
developed by Scorpion shield